“This time next year she won’t remember me,” I thought in the autumn of 2011 when I abandoned my life as an expatriate businesswoman in Dubai to come back to rural Canada to care for my Mom who lived with dementia of the Alzheimer’s type.
After a year she would be placed in a facility where they would take better of her than I could (at least that’s what I imagined), and I’d leave to restart my life somewhere else. That plan was based on what I knew about dementia and dementia care at the time, which was next to nil.
Like most people, I saw Alzheimer disease and other dementias as a terrible tragedy in which those who live with dementia are on a journey that is nothing more than a long slow, tortuous train through hell – a journey in which they are robbed of their very selves as they disappear into a black hole of oblivion. I was mistaken in those beliefs. Today, based on my experience with people who live with dementia, I see the disease and those who have it in a completely different light.
But I was right about one thing. On November 16, 2012, a little over a year after I came back to Canada from Dubai, Mom was placed in a long-term care facility. Once I saw the reality of institutional care, I again abandoned my own life plan to stay close by her side and be her advocate.
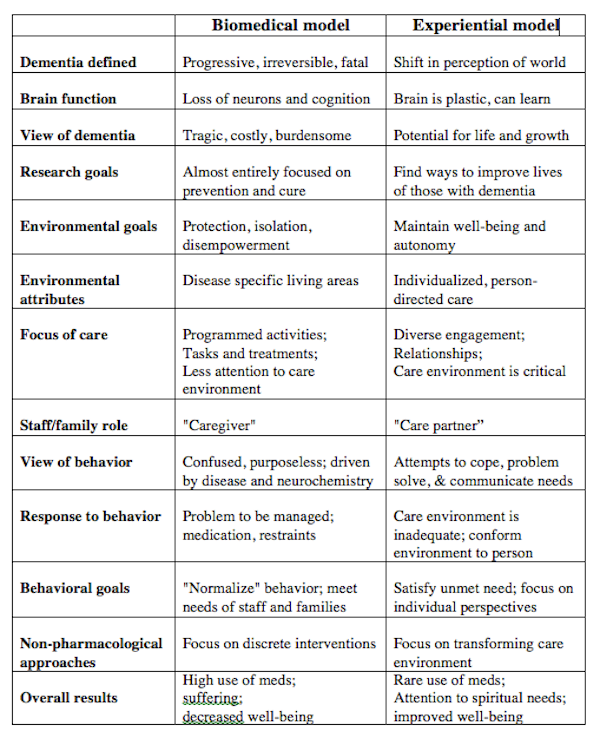
To say that my advocacy was not well received would be an understatement of gargantuan proportions. It took another year before I understood some of the fundamental reasons why the powers that be and I were at such serious odds. The roots of the conflict around my mother’s care lay in perspective, power and control. On the issue of perspective, this chart, from Dr. G. Allen Power’s book “Dementia Beyond Drugs: Changing the Culture of Care,” captures the essence of where experience took me:
When I first read down the right-hand column I found myself nodding in agreement on every point.
My dementia glass is half full. I am 100% sure, based on my own experience, that people with dementia still have great potential for life and growth, they can still learn, and their responsive behaviours are attempts to cope, problem solve and communicate their needs. This is no theory. I know it to be true because I’ve experienced it first hand.
As a result, I am completely convinced that individualized, person-centered living that engages people who live with dementia is critical to their well being. Positive approach to dementia care advocates worldwide share my view; research supports our position.
On the other hand, I suspect that many institutions and people in the medical profession still subscribe to biomedical model that leads to the high use of medications (particularly antipsychotics such Risperdal and Seroquel), and produces needless suffering and decreased well being.
The biomedical model is outdated and out of step with the reality and the needs of people living with dementia as well as their care partners.
It’s time for a change. People living with dementia deserve better. So do the people who walk with them.
Download a pdf of the models chart here.
https://myalzheimersstory.com/2018/05/19/we-need-a-paradigm-shift/
#mc_embed_signup{background:#fff; clear:left; font:14px Helvetica,Arial,sans-serif; }
/* Add your own MailChimp form style overrides in your site stylesheet or in this style block.
We recommend moving this block and the preceding CSS link to the HEAD of your HTML file. */





I definitely vote in favor of Experiential Model and I agree that even that needs be tailored to each individual.
LikeLike
Yes Michael, I’m with you 100%.
LikeLike
Interesting contrast. I have no idea about the practicals of the experimental model, but it looks good and I can say that I would want it if I end up with the Alzheimer’s.
LikeLike
Heidi,
Yes, it’s intellectually interesting and, for those who have dementia, the results mean either thriving or simply surviving.
Those who subscribe to the Biomedical Model might describe people as “suffering” from dementia and say there’s little that can be done but medicate them to ease their pain and address the behavioural and psychological symptoms of dementia (BPSDs).
Proponents of the ExperIENTIAL (not experimental) model would suggest people have the potential to live well with dementia if given the right kind support, environment help to engage life in whatever ways they can until the end. They would say BPSDs are in most cases normal responsive behaviours to the environment and the way others interact with the person living with dementia. More on that in upcoming posts.
LikeLike
Susan, as you are probably aware, I “live” the experiential model! I think Dr. Power’s chart is spot on.
Great blog post!
Best,
Dave
LikeLike
thanks David, yes I know you LIVE the experiential model and that’s why I was keen for you to see the article and share your thoughts. thank you so much. Best in return, Susan
LikeLike
This is very interesting and I’m so happy you and I are collaborating to help care partners understand and implement the experiential model. In my naivety, it surprises me that so many institutions don’t embrace it and that it’s actually a relatively new approach.
LikeLike
Not only do many institution not embrace the experiential model, but they are firmly entrenched in the biomedical model and extremely resistant to change! Sad really…
But maybe we can change all that. No wait, we WILL change all that!
😉
LikeLike
A great article. .. and I too am in favour of the experiential model. The last category i.e. that dealing with the high use of meds, I found extremely appropriate to a recent experience – as follows:
A friend of ours recently underwent a second stroke. They then discovered that he required 3 stents. The 80 year old man, underwent surgery and afterwards exhibited what, to the medical practitioners and nurses was bizarre behaviour… he couldn’t sleep, hallucinated, could not converse intelligibly, refused to stay in his bed etc., etc.
The medicos,( including a neurologist) said that he had dementia, and sedated him with a drug called Ativan (in South Africa) … it may have a different name elsewhere?
I went to see him and he was completely sedated – lying in his hospital bed (almost literally dead to the world!) His daughter was trying to explain to the nursing staff that he did not have dementia; that two days prior he had been conversing with everyone… and apart fro the immediate effects of the stroke was totally copus mentum.
I Added my pennyworth and suggested that he had delirium; that dementia did not present in a matter of a few hours… that the delirium was probably due to the surgery and anesthesia. To cut a long story short; she contacted the neurologist and persuaded him to stop the Ativan. THE VERY NEXT DAY HER FATHER WAS SITTING UP, READING THE NEWSPAPER AND CONVERSING WITH FAMILY AND FRIENDS! (I was told later that the drug itself can sometimes cause the very behaviour for which it was being administered?)
A lot of problems are due ignorance (even amongst specialists who should know better) and medication’s of convenience. I wonder how many people of yesteryear were consigned to mental institutions because of this fact? Thankfully – he is now home and well on his way to recovery.
Henry Spencer
By the way Susan, our recent exchange of viewpoints has been of great assistance to me… I am completing a book on dementia, but have always been a little concerned / confused as to how they should be described.
I am currently in the process of editing it and removing words such as suffering, victim, patient and even wanderers… and wherever possible replacing them with PWD (Person / people with dementia). and other similar non- invasive; non-judgmental forms of address. Thank you for the insights… see you can even teach an old dog new tricks!
.
LikeLike