In mid-2014, I devoured Dr. Allen Power’s first book Dementia Beyond Drugs: Changing the Culture of Care. My tattered copy is full of underlines, stars, tick marks, and highlights. I’ve referred back to it so many times the pages are starting to fall out.
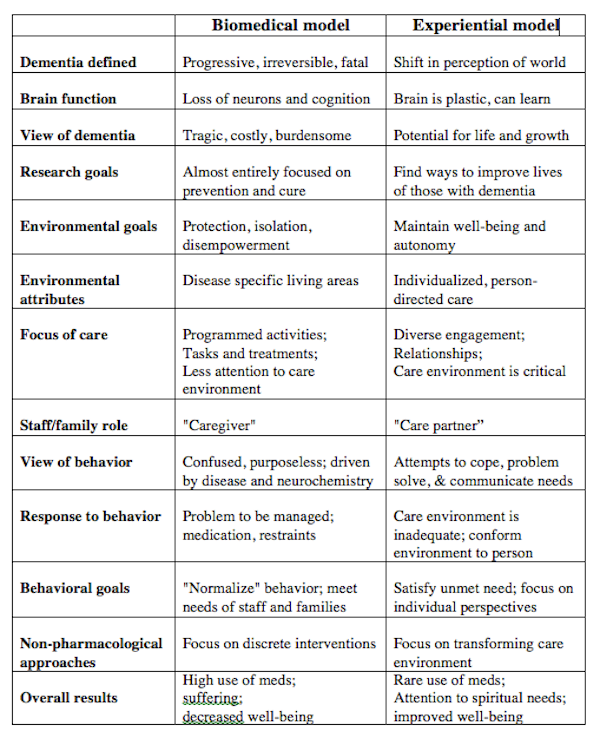
I kick myself for waiting too long to get his second book Dementia Beyond Disease: Enhancing Well-Being, but now that I have it in my hot little hands, I’m eating it up as well. It’s hard to say what I love most about Dr. Power’s work, but I was hooked after I saw his alternative to the biomedical model, which, to be honest, I didn’t even know existed until I read his first book.
We need more forward thinkers and innovators such as Dr. Power, who, with Dementia Beyond Disease, takes another giant step forward and pushes the envelope with respect to care models, well-being, and how we perceive dementia as well as the people who live with it.
Here are 10 pieces of wisdom I’ve extracted from the prologue and first chapter alone:
1 ) We lament the millions of neurons lost to dementia and ignore the many millions that work perfectly well.
2 ) Preserve identity, celebrate personhood, and create meaning in the moment.
3 ) Many people have acquired a special type of wisdom that comes from living with dementia. They have come to see their lives as far from over, for they have had to deal more directly and personally with grief, loss, and the sense of impending death.
4 ) Changing our approach can produce more well-being for people living with dementia than any pill that is available today, or is likely to be available in the foreseeable future.
5 ) Well-being cannot be bottled. It doesn’t come in liquid, capsule or pill form.
6 ) We create living environments based on our view of the world, our daily needs, and our staffing patterns, and expect people whose brains are changing to adapt to them. And when they cannot, we diagnose a “behaviour problem” and medicate them.
7 ) Dementia is a shift in the way a person experiences the world around her/him.
8 ) People with dementia continue to learn new information, incorporate data, and use problem-solving skills to adapt to their changing perceptions.
9 ) Over-medication of people with dementia is not simply a problem in nursing homes; it is a community-wide problem that reflects broad societal views.
10 ) We need to change our minds about people whose minds have changed.
Dr. Power’s books are priced in keeping with their value, and are worth every penny. I can’t recommend them to you highly enough.
https://myalzheimersstory.com/2018/04/30/two-quick-dementia-care-conversation-tips-from-dr-al-power/
https://myalzheimersstory.com/2015/10/10/is-your-dementia-glass-half-empty-or-half-full/
#mc_embed_signup{background:#fff; clear:left; font:14px Helvetica,Arial,sans-serif; }
/* Add your own MailChimp form style overrides in your site stylesheet or in this style block.
We recommend moving this block and the preceding CSS link to the HEAD of your HTML file. */
Subscribe to MAS now & get 5 free PDFs & a page of welcome links:
Take my short survey on behaviour here.
Image copyright: dr911 / 123RF Stock Photo