
“Nursing homes in Canada in general are likely the same. They certainly are in Ontario…appalling. Understaffed, horrible working conditions and getting worse. Pie-in-the-sky government run Ministry of Health and Long-term Care, paid to make rules and laws that are absolutely impossible to meet with the severe under funding and lack of adequate staffing.” Reader comment on: Class action accuses one of Canada’s biggest nursing-home companies of neglecting residents
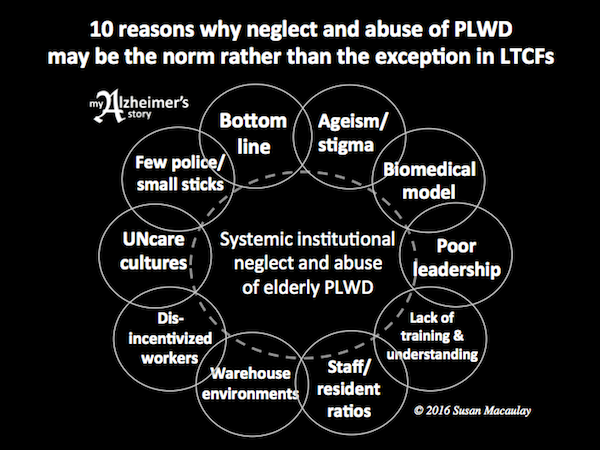
I believe systemic neglect and abuse of elderly people who live with dementia in long-term care facilities is widespread in Canada and around the world. Care workers know about it, nursing home managers and administrators know about it, and some family members of those who are neglected and abused know about it too. Elder neglect and abuse remain pervasive and, worse yet, they are swept under the carpet.
Positive approach to dementia care advocates worldwide are fighting for person-centred care that engages people who live with dementia and helps them to live rich and full lives until the end. Research shows this type of care is essential to the well being of older people, particularly those living with dementia. Treating our elders in any other way is criminal.
Here are some of the factors that allow institutional neglect and abuse to continue:
1 ) Ageism & stigma
Ageist views remain widespread (e.g. old people are useless; their lives don’t matter; our job is to warehouse them, not engage them with life). These unhappy myths negatively impact the way we care for elderly people who live with dementia in their homes, in our communities and in long-term care facilities.
Many people misunderstand the realities of dementia and how it affects those who live with it. Some of the erroneous beliefs include: it doesn’t matter how we treat them; they don’t know what’s happening; they’ll forget in five minutes; they’re not “here” anymore; they don’t understand; they aren’t capable of anything; they are just empty shells; etc. These are myths not truths.
2 ) The biomedical model
Many medical professionals still subscribe to a biomedical model that characterizes dementia as a progressive, irreversible and fatal disease which is tragic, costly and burdensome. Proponents of the model see expressive behaviour as confused, purposeless, and disease driven, manageable only with medication and physical restraints. In fact, it’s proven that reducing the use of antipsychotic drugs in LTCFs increases the well-being of residents living with dementia. The biomedical perspective is dangerous, antiquated and out of step with the reality and the needs of people who live with dementia (PWLD). We must adopt more sophisticated and compassionate approaches that put people at the top of the care pyramid or at the centre of the care circle.
3 ) Poor leadership
Senior executives and medical professionals who manage LTCFs are responsible in large part for most of the factors that follow and for the neglect and abuse that result. Being willing to take a hard look at what has been wrong and what is wrong with failing eldercare organizations and systems takes courage. Identifying shortcomings and fixing them is a gargantuan task that takes vision, will, energy and commitment. If those kinds of people were in leadership positions now, we wouldn’t find ourselves with the existing situation: broken facilities full of broken people.
4 ) Lack of training/understanding
The standard of care in any given facility is only as good as the front line workers who deliver it. Dementia care requires specialized training and understanding; if care workers don’t have the skills they need, neglect and abuse are inevitable. Frontline care staff need the encouragement and support of competent, compassionate, visionary leaders to get the job done.
5 ) Low staff-to-resident ratios
How can one care worker attend to the needs of eight to ten or even more PLWD and do it to a reasonable standard? It’s not possible. And yet, those are the kinds of care worker to resident ratios that prevail in most LTCF. It’s no wonder neglect and abuse are pervasive.
6 ) Warehouse-like environments
There have been recent innovations in design including dementia villages, small group homes, and facilities in which childcare and eldercare are combined. While these approaches have proven successful, organizations that apply them are still relatively few and far between. Most facilities are not designed to meet resident needs, but rather to maximize operational efficiency. Calling a warehouse a “village,” a “manor,” or a “specialized memory care unit,” does not change the essence of what it is.
7 ) Dis-incentivized workers
Care workers tend to be poorly trained and poorly paid, and overworked because of low staff to resident ratios; they are often ill treated, and unappreciated. Further, because they are not properly trained and don’t have the skills they require to interact effectively with PLWD, they tend to produce instead of reduce challenging behavioural expressions that wouldn’t be there if there were more staff, better training, better understanding, suitable environments, engaging activities, etc. It’s a vicious circle.
8 ) NONcare cultures
All of the factors above lead to UNcare cultures in which profits come first, people come last and the status quo is never questioned, or, if and when it is, complainers and whistleblowers are quickly silenced, dismissed, or disavowed. Staff become demoralized, complacent, cynical and hardened to preserve their own sanity. Negative UNcare culture that has become entrenched is hard to change.
9 ) Few “police;” small “sticks”
Regulatory bodies may be stretched beyond capacity. Substandard operations/practices may be difficult to identify because of the way inspections are done (e.g. prior notice of visits results in things being “spit and polish” for inspecting eyes), and offending institutions may remain open and operating despite substandard performance and long lists of regulation breaches and/or regulatory infractions.
10 ) The bottom line
Cost-saving, cost-cutting, and the pursuit of profit are deemed more important than providing vulnerable elders with the care they need and deserve. Residents and families are powerless to change the system to which they have fallen victim.
It’s time to take a closer look at this tragic and completely unacceptable state of affairs, demand research into the nature and prevalence of neglect and abuse in long-term care, and most important, to immediately implement steps stop it. Class action suits such as these are a step in the right direction.
Take my short survey on behaviour here.
Image copyright: warrengoldswain / 123RF Stock Photo




This is a powerful post, with a lot to digest. Points 6 & 7 stood out for me; in the near future, there will be many businesses “competing” for our seniors’ retirement funds. So sad. We will need to be the watch-dogs for our parents, spouses and friends with dementia…. ensuring that they or their families are not overly influenced by exaggerated marketing claims and slick websites with flowery promises. Quality of life is not measurable by data, and numbers mean nothing when it comes to compassion.
The staff in these residences have to take some responsibility as well; but they need education and assistance in doing so, preferably by a community which supports their efforts, even if the capitalistic owners and politically-driven government officials do not. Of course, if we don’t value them, why should they be motivated to improve? You’re right about this being a vicious circle, if not a domino effect. Push the family member too far, and you’ve got an unhappy senior in a residence. Push the staff too far, and you’ve got an unhappy worker along with the unhappy senior. Push the senior too far, and you’ve got everyone getting a little nervous. If we give our seniors the support they need in the first place, we don’t have to get to the last place anyone wants to be…
LikeLike
“Quality of life is not measurable by data, and numbers mean nothing when it comes to compassion.”
Yes, you are SO right. One of the tough issues at the core of all of this is how DO we measure quality of life and how DO we ensure people are being engaged and not neglected and abused? I think you will find the follow-up to this post equally interesting. Stay tuned 🙂
“You’re right about this being a vicious circle, if not a domino effect. Push the family member too far, and you’ve got an unhappy senior in a residence. Push the staff too far, and you’ve got an unhappy worker along with the unhappy senior. Push the senior too far, and you’ve got everyone getting a little nervous. If we give our seniors the support they need in the first place, we don’t have to get to the last place anyone wants to be…”
Bingo again! Vicious Circle + Domino Effect = Downward Spiral 😦
We must look at and address the “system” and the ways in which all the players and factors interact. It’s extremely complex.
LikeLike
Excellent post Lorrie. May I ask if you are in the US? Your point about future competition for the baby boomer’s retirement $ is spot on. This fact should get organizations like AARP, along with voters, to demand that our elected officials be forward thinking and not wait until it becomes a “predicted epidemic” before acting on this upcoming disaster.
When men returned from WWII, housing was built quickly and efficiently to care for our veterans and their blossoming families. Free College was given to returning Vets under the GI bill to train and ultimately create a post war business environment for the future. The idea that our country can’t adapt to this same increase in the aging population quickly is simply not true. We need some of the same broad thinking that was done when large numbers of Americans flooded the country’s infrastructure and it should be apply that to the aging issue.
Offer free schooling for those who would train in specialized dementia care. A 1 yr course vocational – hands on course – dedicated to teaching all the things that Susan and others have shown us that work without drugging our elderly.
Does anyone remember the Peace Corp and the young people who trained for deployment? There was a sense of pride that went with this training and the work that they would be doing for the needy. We need to have others see how important the work of caring for our elderly and dementia patients is and recognize that specialized training the same as we do for Firemen and Police. We honor our first responders and pay them for the stress their jobs create. Why not suggest that the workers in dementia environments are just as important and need to be trained just as we do for our other important community positions?
When people are placed in jobs that are looked at as lowly and untrained they tend to live up to those expectations and those jobs attract truly untrained and sometimes cruel people. Let’s place the value on our elderly’s caretakers that show that we respect and care for our aging population, including ourselves one day.
Wouldn’t it be nice to believe that when we retire and possibly are mentally unable to care for ourselves, that we will be placed in a loving environment where our dignity will be honored until death visits us? I want to believe it can be done – and can be done swiftly like we did when our vets returned from the war. It doesn’t have to be an imagined Utopia.
LikeLike
Hi Connie – Thanks for all the information about returning vets and the Peace Corp, that was interesting! Like Susan, the author of this post, I’m in Canada, not the USA. And being quite cynical, may I suggest that the government is much more motivated to help people who are in the public eye – although I’ve heard horror stories about the way our vets are treated when they need medical assistance, so there are conflicting stories, I assume? But the government knows that they need soldiers, firemen and police in order to safeguard a country, so – again – they are highly motivated to treat them well. Seniors are, for all capitalistic intents and purposes, of no use to anyone. There is no motivation beyond the humane, compassionate one to treat them well. That said, I totally agree with you that we SHOULD be able to expect fair treatment at the end of our lives, and especially if we are mentally unable to care for ourselves. Let’s keep the discussion going and see if we can effect changes in both countries!
LikeLike
Well said Lorrie and I also appreciate Connie’s storytelling abilities.
LikeLike
Beautifully written and thanks for your thoughts Connie ❤
LikeLike
With everything said + done. How can I prevent this or to whom can we address this cycle to? I visit my husband everyday at least 6 days a week for the last 4 years. In my heart I want to keep him home but now he can’t rise up from the wheelchair. Since he’s been there for rehab, he only got worse. Please keep me posted.
LikeLike
Myrna, I’m sorry for the challenges you and your husband are facing. Sometimes it can be difficult, if not impossible to make change. That said, depending on where you are, you may be able to get outside authorities such as ombudsmen involved in your situation. I’m sure the fact that you are with him virtually every day brings comfort to your husband and that at least is a good thing.
LikeLike
Excellent conversation Older people’s councils established in each county in Ireland are charged with making their area age friendly. This includes looking at care of the elderly listening to them and we will be looking at care in nursing homes their medication policies and what activities they are providing Groups like Avtive Retirement associations can contribute to knowledge and initiatives in this field Each local area need to look at all aspects of Age Friendly Practices
LikeLike
intentional IGNORANCE is an excuse for MEANNESS
if a nurse intentionally does NOT know a HOT DAY can cause DEHYDRATION
than the nurse will NOT give more WATER to the residents
and if a resident die because of DEHYDRATION
the excuse is always: she is really sick anyway
at least now , she is not suffering !!
LikeLike