On December 3, 2013, a year after Mom had moved into a long-term care facility (LTCF), I sent an email to the person in legal control of my mother’s care, and the Director of Nursing of the LTCF. It read in part:
I am deeply distressed by Mom’s present condition.
I have reviewed in detail the nurses’ notes from November 2012 to September 2013. Based on the notes and my own observations of Mom’s health and behaviour, I’m convinced the well-intentioned strategy of medicating Mom more and more is not the best way forward. These are some of the deleterious effects I see:
- Her balance and ability to walk are being affected, thus increasing the likelihood of falls and injury
- Her quality of life is diminished
- Her capacity to enjoy life is diminished
- Her dignity is being compromised rather than preserved
- She is gaining a great deal of weight
- Her decline is being accelerated
Two simple actions will immediately alleviate the problem:
- provide one-on-one care to Mom from 09:00 – 21:00 seven days per week
- reduce the Seroquel and Risperdal she is being given
Moving her to the second floor to a room of her own will also help.
I would like to work together to determine what combination of medication, dosages, activities, and one-on-one care levels best meet Mom’s needs and allows her to enjoy life in whatever way she can in her remaining time, while also respecting the rights of other residents and staff.
The Director of Nursing, the on-call facility doctor to whom Mom had been assigned (and who had likely seen her for less than an hour in total over the previous year), the person in legal control of Mom’s care (plus spouse), and I met the following week.
During that meeting, I was told I didn’t understand my mother’s disease or her behaviour, that she could not have additional one-on-one care for several arbitrary reasons, that she had to be medicated for the safety of others, and that if I didn’t stop asking questions about her care we would need to find her another home.
At that point, I had not yet read Dr. Allen Power’s book Dementia Beyond Drugs, or Naomi Feil’s book The Validation Breakthrough. I didn’t know about the biomedical or experiential models; I hadn’t been exposed to the mountain of evidence that clearly demonstrates the inefficacy of antipsychotic medications in treating people who live with dementia; and I hadn’t yet fully grasped the fact that the behaviours labeled “challenging” in people who live with dementia are actually normal human responses to care approaches, unmet needs, environmental conditions and psycho-social circumstances.
But I knew with 100% certainty that what was happening to my mother was cruel, unnecessary and abusive, and that there was a better way. I knew it at the very core of my being.
Less than two months later, during court proceedings I had initiated to try to gain control of my mother’s care so I could get her out of ElderJail, the same doctor repeated essentially the same things he had said in our December meeting. He also told the judge that a “chemical belt” comprising the antipsychotics quetiapine (Seroquel) and risperidone (Risperdal) was “really a good thing,” because it “protects” people living with Alzheimer disease and “gives them a good quality of life.”
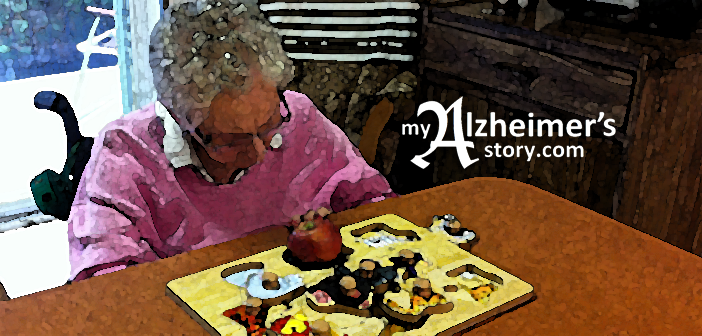
He didn’t clarify what he meant by “quality of life,” and he knew virtually nothing about my mother. Here she is at 10:23 on December 1, 2013, experiencing the effects of Seroquel and Risperdal — effects which lasted for four to five hours every day:
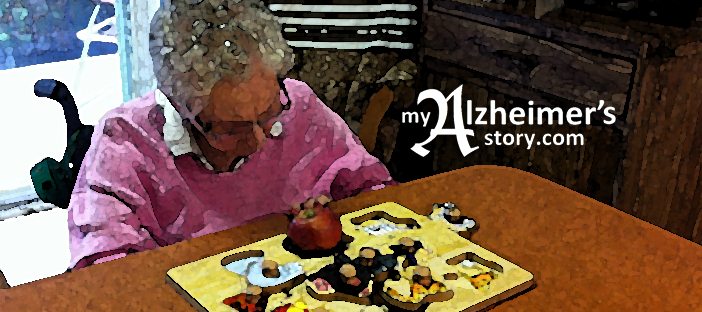
For comparative purposes, here’s Mom in the late afternoon (after that day’s meds had mostly worn off) during a music therapy session I arranged for her a few weeks later:
I lost my bid to get legal control of my mother’s care, and she was inappropriately medicated with Seroquel and Risperdal until she died in August 2016.
Alzheimer’s disease didn’t rob my mother of her self, antipsychotics did. Giving her these drugs caused her to lose her ability to walk, to fall repeatedly until she was confined to a wheelchair, to exist in a catatonic state for hours every day, and to develop tardive dyskinesia. They stopped her from engaging with life in the way she wanted during her last four years.
I repeatedly requested that the drugs be stopped; I was ignored or admonished. Worse, Mom and I were both punished for my advocacy: the time we were allowed to spend together was reduced to between 1 and 3 p.m. (when she was usually “asleep”) for the final 18 months of her life. This under threat of denying me access to her completely.
Underlying this tragedy is the “drug culture,” and broken eldercare system that prevail in the province of Quebec, where I live, and where 40 to 60% of elders in LTCFs are given antipsychotic medications, the vast majority of whom do not have a diagnosis of psychosis and are therefore being inappropriately medicated just like Mom was. The Quebec rate of prescribing antipsychotics to people with dementia in LTC is about double the 25% national average. This video shows the overall use of antipsychotics in the elderly in Quebec compared with the rest of Canada:
Having failed to get them to stop giving Mom antipsychotics, I did whatever I could to bring her happiness. I visited her every day, and created as many joyful moments for the two of us as I could, even though I felt as if I were watching her being slowly tortured to death every time I saw her.
At the same time, I continued to advocate for better care for her and for others who live with dementia. Among other things, I produced and shared the animated graph above, I blogged about the situation in the province; I wrote an open letter to the provincial Minister of Health, Gaétan Barrette, about neglect; I spoke out against the inappropriate use of antipsychotics in dementia care worldwide; I shared my story with a standing committee of the Canadian Senate, connected with like-minded pioneers around the world and had two articles accepted for publication in the Journal of the American Medical Directors Association.
But systemic change doesn’t come easy.
Then, on November 30, 2017, four years after the email with which I began this piece, the Minister of Health announced the launch of an initiative in partnership with the Canadian Foundation for Healthcare improvement (CFHI) to reduce the use of antipsychotics in the Quebec’s LTCFs. The CFHI does amazing work.
Here’s a partial translation of a French-language article, which appeared in LaPresse about the project:
On Thursday November 30, Quebec’s Minister of Health, Gaétan Barrette, announced the launch of a province-wide project to reduce the use of antipsychotics in long-term care facilities (LTCFs / CHSLD). The project will initially comprise 24 LTCFs, and will be rolled out over three years to 317 of the 400 LTCFs in the province.
“There is no doubt that there is overuse [of antipsychotics]. So, in the end, there must be a reduction,” said the minister during a media scrum.
Antipsychotics are frequently prescribed in LTCFs to “chemically restrain” residents in to avoid having to physically do so. The medications calm or sedate, and thus restrain the person “pharmacologically” rather than physically.
“Many people criticize chemical restraints,” acknowledged the minister. “I am not saying that antipsychotics will no longer be used, but we accept that there are probably too many [being prescribed]. We want to reduce them to what is really necessary.”
The project is being undertaken jointly with the Canadian Foundation for Healthcare Improvement (CFHI), which piloted it in 56 long-term care facilities in eight provinces in 2014/15 with astonishing results. Most important, said CFHI President and CEO Maureen O’Neill, is that patients recovered some of their identity: “The families of residents who are weaned from the antipsychotics they were inappropriately taking say they get back loved ones they thought they had lost forever,” she said.
The CFHI notes that people are becoming increasingly aware of the problem of over-prescription of antipsychotic medication to the elderly in long-term care. Five years ago, on average in Canada, 32% of residents of LTCFs were prescribed antipsychotics; that has since been reduced to 23.9% thanks to initiatives such as this one. In Quebec by comparison, between 40% and 60% of people aged 65 and over living in LTCFs are prescribed antipsychotics without having been diagnosed with psychosis.
I wept when I read the story in LaPresse. I wept for the pain Mom and I suffered because of ignorance, pride and greed, as well as others’ needs for power and control. But I refuse to let our experience be without meaning or purpose. I choose to believe that my advocacy played a part in generating the energy for this initiative that will positively impact tens of thousands of elderly people living with dementia in Quebec’s LTCFs in the future.
It’s too late for my mom. But it’s not too late for others.
https://myalzheimersstory.com/2019/06/07/just-like-one-flew-over-the-cuckoos-nest/
https://myalzheimersstory.com/2016/07/26/40-side-effects-of-seroquel/
https://myalzheimersstory.com/2017/12/09/30-haloperidol-haldol-side-effects/
#mc_embed_signup{background:#fff; clear:left; font:14px Helvetica,Arial,sans-serif; }
/* Add your own MailChimp form style overrides in your site stylesheet or in this style block.
We recommend moving this block and the preceding CSS link to the HEAD of your HTML file. */
Subscribe to MAS now & get 5 free PDFs & a page of welcome links:
//s3.amazonaws.com/downloads.mailchimp.com/js/mc-validate.js(function($) {window.fnames = new Array(); window.ftypes = new Array();fnames[0]=’EMAIL’;ftypes[0]=’email’;fnames[1]=’FNAME’;ftypes[1]=’text’;fnames[2]=’LNAME’;ftypes[2]=’text’;}(jQuery));var $mcj = jQuery.noConflict(true);



Susan, you have done marvellous work for your mother and for the mothers, fathers, uncles, aunts who will benefit from your advocacy. I empathize with your frustration with the systemic responses and cannot imagine the pain you experienced during those last 18 months and before. Thank you for sharing your stories.
LikeLike
Thanks so much Bonny. it’s my purpose to use this experience to help others, so it’s really gratifying to hear that my advocacy is making a difference – but it surely is a long row to hoe!
LikeLike
It is a long road to hoe; thank you again for your labour, it is so important. Merry Christmas to you and all the best over the holidays and the new year. Stay brave and keep doing this work as long as you can-you have done so much!
LikeLike
Thanks again @Bonny and Merry Christmas to you too ❤
LikeLike
Susan, you are an extraordinary person. Not only have you saved other elders from a horrible fate but you have touched me and I’m sure others. You provide hope, inspiration and support to those of us out there care giving. Keep up the fight and inspiration. Please know you get me through those tough days. I thank you for sharing your strength and knowledge.
LikeLike
Hello,
I lost my mother less than 3weeks ago on June 23. Your story resonates with me bc I believe a combination of factors, including the overuse of medications were responsible for her rapid decline in only 7months. When she was assessed as combative during shower days the answer was to increase her Respirodone. She moved into LTC in December and lived only 7months. Our system is failing our elderly with dementia and changes need to happen. Your continued advocacy and work is so important.
LikeLike
Martha, I’m so sorry for the loss of your mother, particularly under the circumstances you describe. Stories like yours (and mine!) Make me even more determined to create positive change. Suffering is bad enough, but needless suffering is even worse. I hope you can find a way to turn your experience into something positive in honour of your mom ❤
LikeLike
Your story breaks my heart. My dad died suddenly, and when we realized she had dementia and he had been covering for her, she was suffering from malnutrition, and her power was almost shut off during the winter because she wrote checks to pay bills (sometimes 2-3 times) but didn’t mail them. It was a scary time.
I know things aren’t the same everywhere as they are in the US, but I urge your US readers to get medical power of attorney from aging loved ones BEFORE they are too far gone to consent. This gives you control of the medical decisions being made. Some wise person told me this, and because of it, I am able to exercise a lot more control over such things.
LikeLike
Thanks Ellen, that’s great advice, which I share all the time. Sadly, people still end up in a pickle 😦
And thanks for your kindness and compassion.
Susan
LikeLike